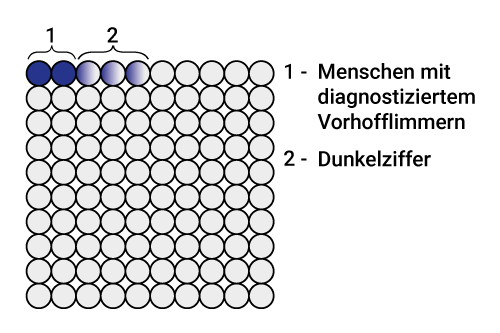
Case numbers and hidden numbers
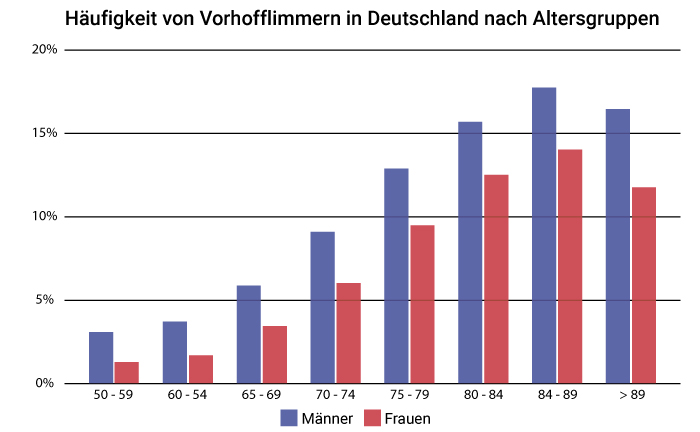
Atrial fibrillation has long since become a widespread disease in Germany. More and more people suffer from atrial fibrillation, often unnoticed. The chance of developing atrial fibrillation is particularly high in old age. This, in combination with the demographic development in Germany, is the reason for the increasing number of cases. Men are more likely to develop the disease than women.
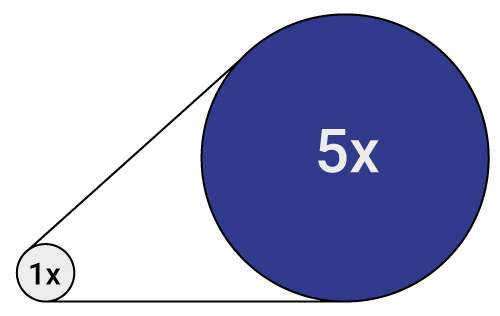
About 5% of the German population suffers from atrial fibrillation. That corresponds to about 4,000,000 people. However, only about 1,600,000 people, which is less than half of those affected, have been diagnosed. Often, atrial fibrillation remains asymptomatic and thus undetected. Sudden ischaemic strokes, supposedly without cause, are the result.
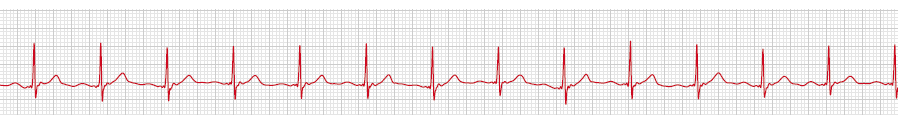
That is why it is advisable to specifically look for atrial fibrillation in old age, and do a so-called screening. Experts advise taking an ECG for 72 hours, even if no symptoms of atrial fibrillation are known or no abnormalities were seen in the resting ECG. In this way, a reliable risk profile can be created for each patient.
Based on this risk profile, which should also take into account other risk factors such as blood pressure, obesity and previous illnesses, the number of possible patients has risen to over 20,000,000 in Germany alone.